Search
- Page Path
- HOME > Search
Response
- Diabetes, Obesity and Metabolism
- Characteristics of Glycemic Control and Long-Term Complications in Patients with Young-Onset Type 2 Diabetes (Endocrinol Metab 2022;37:641-51, Han-sang Baek et al.)
- Han-sang Baek, Ji-Yeon Park, Jin Yu, Joonyub Lee, Yeoree Yang, Jeonghoon Ha, Seung Hwan Lee, Jae Hyoung Cho, Dong-Jun Lim, Hun-Sung Kim
- Endocrinol Metab. 2022;37(6):945-946. Published online December 2, 2022
- DOI: https://doi.org/10.3803/EnM.2022.602
- [Original]
- 1,783 View
- 165 Download

Original Articles
- Diabetes, Obesity and Metabolism
- Characteristics of Glycemic Control and Long-Term Complications in Patients with Young-Onset Type 2 Diabetes
- Han-sang Baek, Ji-Yeon Park, Jin Yu, Joonyub Lee, Yeoree Yang, Jeonghoon Ha, Seung Hwan Lee, Jae Hyoung Cho, Dong-Jun Lim, Hun-Sung Kim
- Endocrinol Metab. 2022;37(4):641-651. Published online August 29, 2022
- DOI: https://doi.org/10.3803/EnM.2022.1501
- 6,257 View
- 166 Download
- 10 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
The prevalence of young-onset diabetes (YOD) has been increasing worldwide. As the incidence of YOD increases, it is necessary to determine the characteristics of YOD and the factors that influence its development and associated complications.
Methods
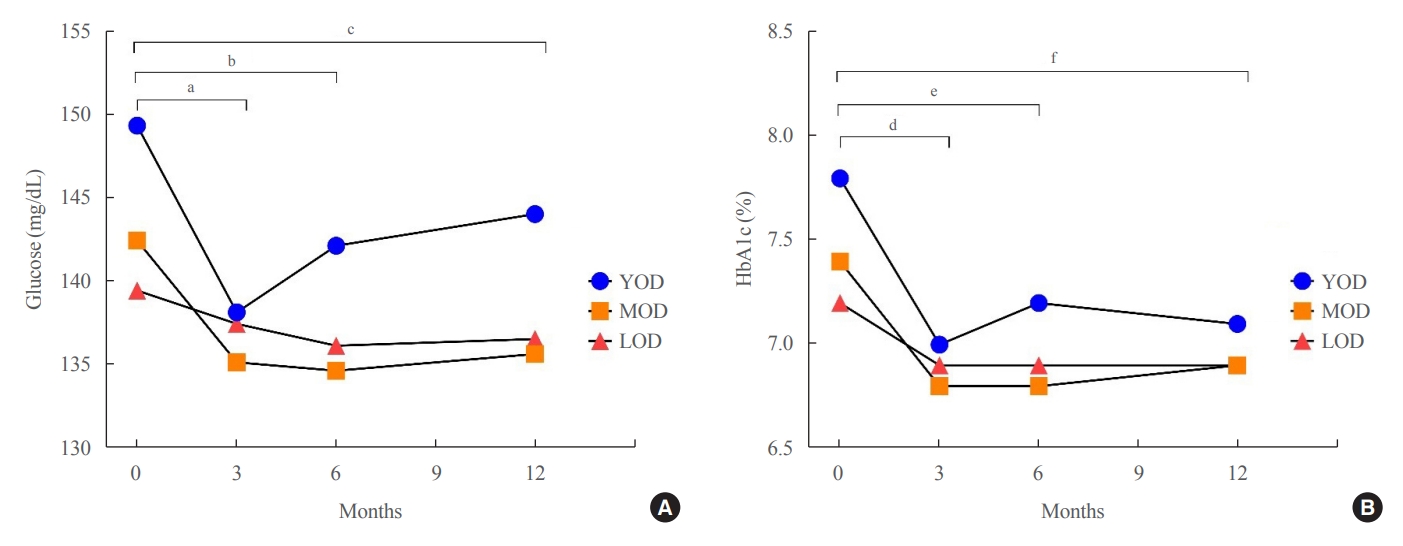
In this retrospective study, we recruited patients who were diagnosed with type 2 diabetes mellitus between June 2001 and December 2021 at a tertiary hospital. The study population was categorized according to age: YOD (age <40 years), middle-age-onset diabetes (MOD, 40≤ age <65 years), and late-onset diabetes (LOD, age ≥65 years). We examined trends in glycemic control by analyzing fasting glucose levels during the first year in each age group. A Cox proportional-hazards model was used to determine the relative risk of developing complications according to glycemic control trends.
Results
The fasting glucose level at the time of diagnosis was highest in the YOD group (YOD 149±65 mg/dL; MOD 143±54 mg/dL; and LOD 140±55 mg/dL; p=0.009). In the YOD group, glucose levels decreased at 3 months, but increased by 12 months. YOD patients and those with poor glycemic control in the first year were at a higher risk of developing complications, whereas the risk in patients with LOD was not statistically significant.
Conclusion
YOD patients had higher glucose levels at diagnosis, and their glycemic control was poorly maintained. As poor glycemic control can influence the development of complications, especially in young patients, intensive treatment is necessary for patients with YOD. -
Citations
Citations to this article as recorded by- Increased risk of incident mental disorders in adults with new-onset type 1 diabetes diagnosed after the age of 19: A nationwide cohort study
Seohyun Kim, Gyuri Kim, So Hyun Cho, Rosa Oh, Ji Yoon Kim, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Jae Hyeon Kim
Diabetes & Metabolism.2024; 50(1): 101505. CrossRef - Association between age at diagnosis of type 2 diabetes and cardiovascular morbidity and mortality risks: A nationwide population-based study
Da Hea Seo, Mina Kim, Young Ju Suh, Yongin Cho, Seong Hee Ahn, Seongbin Hong, So Hun Kim
Diabetes Research and Clinical Practice.2024; 208: 111098. CrossRef - Impact of diabetes distress on glycemic control and diabetic complications in type 2 diabetes mellitus
Hye-Sun Park, Yongin Cho, Da Hea Seo, Seong Hee Ahn, Seongbin Hong, Young Ju Suh, Suk Chon, Jeong-Taek Woo, Sei Hyun Baik, Kwan Woo Lee, So Hun Kim
Scientific Reports.2024;[Epub] CrossRef - Early onset type 2 diabetes mellitus: an update
Myrsini Strati, Melpomeni Moustaki, Theodora Psaltopoulou, Andromachi Vryonidou, Stavroula A. Paschou
Endocrine.2024;[Epub] CrossRef - Complications and Treatment of Early-Onset Type 2 Diabetes
Fahimeh Soheilipour, Naghmeh Abbasi Kasbi, Mahshid Imankhan, Delaram Eskandari
International Journal of Endocrinology and Metabolism.2023;[Epub] CrossRef - Characteristics of Glycemic Control and Long-Term Complications in Patients with Young-Onset Type 2 Diabetes (Endocrinol Metab 2022;37:641-51, Han-sang Baek et al.)
Han-sang Baek, Ji-Yeon Park, Jin Yu, Joonyub Lee, Yeoree Yang, Jeonghoon Ha, Seung Hwan Lee, Jae Hyoung Cho, Dong-Jun Lim, Hun-Sung Kim
Endocrinology and Metabolism.2022; 37(6): 945. CrossRef -
ISPAD
Clinical Practice Consensus Guidelines 2022: Management of the child, adolescent, and young adult with diabetes in limited resource settings
Anju Virmani, Stuart J. Brink, Angela Middlehurst, Fauzia Mohsin, Franco Giraudo, Archana Sarda, Sana Ajmal, Julia E. von Oettingen, Kuben Pillay, Supawadee Likitmaskul, Luis Eduardo Calliari, Maria E. Craig
Pediatric Diabetes.2022; 23(8): 1529. CrossRef - Characteristics of Glycemic Control and Long-Term Complications in Patients with Young-Onset Type 2 Diabetes (Endocrinol Metab 2022;37:641-51, Han-sang Baek et al.)
May Thu Hla Aye, Sajid Adhi Raja, Vui Heng Chong
Endocrinology and Metabolism.2022; 37(6): 943. CrossRef
- Increased risk of incident mental disorders in adults with new-onset type 1 diabetes diagnosed after the age of 19: A nationwide cohort study

- Prevalence and Characteristics of Metabolically Obese but Normal Weight and Metabolically Healthy but Obese in Middle-aged Koreans: the Chungju Metabolic Disease Cohort (CMC) Study.
- Seung Hwan Lee, Hee Sung Ha, Young Jun Park, Jin Hee Lee, Hyeon Woo Yim, Kun Ho Yoon, Moo Il Kang, Won Chul Lee, Ho Young Son, Yong Moon Park, Hyuk Sang Kwon
- Endocrinol Metab. 2011;26(2):133-141. Published online June 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.2.133
- 2,393 View
- 35 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
We attempted to determine the prevalence and characteristics of metabolically obese but normal weight (MONW) and metabolically healthy but obese (MHO) individuals in a large cohort of middle-aged Koreans. METHODS: 8,987 non-diabetic subjects were selected from the Chungju Metabolic disease Cohort Study performed in 2003-2006. MONW was defined as a body mass index (BMI) > or = 18.5 and < 23 kg/m2 with a homeostasis model assessment of insulin resistance (HOMA-IR) in the highest quartile. MHO was defined as BMI > or = 25 kg/m2 with HOMA-IR in the lowest quartile. RESULTS: The mean age of the subjects was 62.3 +/- 10.5 years (men 40.4%). The age-adjusted prevalence of MONW and MHO were 4.3% (5.3% men, 3.7% women) and 5.6% (3.6% men, 7.0% women), respectively. 14.2% of men and 12.9% of women were classified as MONW among the normal weight population, whereas 10.7% of men and 14.5% of women were classified as MHO among the obese subjects. The prevalence of prediabetes was significantly higher in the MONW group than in the MHO group (34.7 vs. 12.5%, P < 0.0001 in men; 23.1 vs. 8.8%, P < 0.0001 in women). The MONW group evidenced an equivalent risk of coronary heart disease (CHD) relative to the MHO group (10.77 +/- 0.68 vs. 10.22 +/- 0.90% in men; 7.02 +/- 0.34 vs. 7.26 +/- 0.26% in women, means +/- standard error [SE]). CONCLUSION: The subjects in the MONW group are characterized by a high risk of diabetes and CHD, despite their normal weights. Their substantial prevalence in the population emphasizes the importance of identifying subjects in the MONW group, and warrants more intensive risk management. -
Citations
Citations to this article as recorded by- Obesity, metabolic health, and mortality in adults: a nationwide population-based study in Korea
Hae Kyung Yang, Kyungdo Han, Hyuk-Sang Kwon, Yong-Moon Park, Jae-Hyoung Cho, Kun-Ho Yoon, Moo-Il Kang, Bong-Yun Cha, Seung-Hwan Lee
Scientific Reports.2016;[Epub] CrossRef - The Definition of Metabolically Healthy Obesity
Hae Kyung Yang, Seung-Hwan Lee
The Journal of Korean Diabetes.2014; 15(1): 17. CrossRef
- Obesity, metabolic health, and mortality in adults: a nationwide population-based study in Korea

Case Reports
- A Case of Incidentally Diagnosed Adrenal Paragonimiasis.
- Shin Ae Park, Seung Hwan Lee, Seung Hyun Ko, Jun Gi Kim, Soo Youn Park, Jin Young Yoo, Ho Woo Nam, Yu Bae Ahn
- Endocrinol Metab. 2011;26(1):97-100. Published online March 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.1.97
- 1,857 View
- 23 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - We report here on a rare case of adrenal paragonimiasis that presented with an adrenal incidentaloma. A 52-year-old male presented with fatigue and weight loss. The laboratory findings revealed eosinophilia (8.5%) and an increased eosinophil count (910/microL). The computed tomography scan showed 6.5 x 5 cm sized multilocular cystic mass in the right adrenal gland, which was non-functioning, and cystic lesions with variable sizes were also noted in the abdominal cavity. On the surgical field, whitish patches were spread out in the peritoneum, the omentum, the dome of the liver and the diaphragm. The right adrenal gland was replaced by a cystic mass filled with mucopurulent creamy materials. The pathologic findings revealed numerous eggs of Paragonimus spp. Also, the ELISA was positive for IgG paragonimus antibody. The adrenal gland can become infected by various microbial pathogens, including parasites, although it is relatively uncommon. However, in the case of a cystic adrenal mass with accompanying eosinophilia in an endemic area, clinicians should consider the possibility of parasitic infection.
-
Citations
Citations to this article as recorded by- Paragonimus westermani infection manifesting as a pulmonary cavity and adrenal gland mass: A case report
Yong Shik Kwon, Hye Won Lee, Hyun Jung Kim
Journal of Infection and Chemotherapy.2019; 25(3): 200. CrossRef - A Case of Ectopic Peritoneal Paragonimiasis Mimicking Diverticulitis or Abdominal Abscess
Min Jae Kim, Sung-Han Kim, Sang-Oh Lee, Sang-Ho Choi, Yang Soo Kim, Jun Hee Woo, Yong Sik Yoon, Kyung Won Kim, Jaeeun Cho, Jong-Yil Chai, Yong Pil Chong
The Korean Journal of Parasitology.2017; 55(3): 313. CrossRef - Paragonimiasis in the Abdominal Cavity and Subcutaneous Tissue: Report of 3 Cases
Chang Ho Lee, Jong Hun Kim, Woo Sung Moon, Min Ro Lee
The Korean Journal of Parasitology.2012; 50(4): 345. CrossRef
- Paragonimus westermani infection manifesting as a pulmonary cavity and adrenal gland mass: A case report

- A Case of Ectopic Neurohypophysis Presenting with Hypogonadism.
- In Woon Baek, Ji Hyun Kim, Guk Jin Lee, Kyoung Eun Lee, Hae Lim Lee, Hye Won Lee, Nam Yong Kim, Yon Kwon Ihn, Seung Hyun Ko, Seung Hwan Lee, Je Ho Han
- Endocrinol Metab. 2011;26(1):67-71. Published online March 1, 2011
- DOI: https://doi.org/10.3803/EnM.2011.26.1.67
- 2,226 View
- 27 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Pituitary stalk interruption and ectopic neurohypophysis seen on magnetic resonance Imaging (MRI) are often associated with either isolated growth hormone (GH) deficiency or combined anterior pituitary hormone deficiency, but their pathogenesis is not clear and the clinical data regarding these anatomical defect is limited. We experienced a 23-year-old male with the absence of secondary sexual characteristics and this was accompanied with pituitary stalk dysgenesis and ectopic neurohypophysis. He received growth hormone for a year when he was 12 years old due to his short stature. Sella MRI showed no visible pituitary stalk with minimal high signal change, suggesting ectopic neurohypophysis. The combined pituitary stimulation test revealed blunted responses of growth hormone, follicle stimulating hormone and luteinizing hormone. For the hypogonadotropic hypogonadism, the patient was given testosterone intramuscularly and he gradually developed secondary sexual characteristics. We concluded that the hypogonadism and growth hormone deficiency in this patient was caused by hypopituitarism due to pituitary stalk dysgenesis and ecopic nuerohypophysis.
-
Citations
Citations to this article as recorded by- MRI of ectopic posterior pituitary gland with dysgenesis of pituitary stalk in a patient with hypogonadotropic hypogonadism
Ashim Kumar Lahiri, Ramanivas Sundareyan, David Jenkins, Anjumara Nilak
Radiology Case Reports.2018; 13(4): 764. CrossRef - Hypothalamic Hypopituitarism Caused by Pituitary Stalk Dysgenesis
Seong-Ju Lee, Hye-Jin Yoon, A-Reum Cho, Yoo-Jin Um, Keun-Young Park, Dong-Mee Lim, Byung-Joon Kim
Korean Journal of Medicine.2013; 85(4): 420. CrossRef
- MRI of ectopic posterior pituitary gland with dysgenesis of pituitary stalk in a patient with hypogonadotropic hypogonadism

- A Patient with Primary Amyloidosis Misrecognized as Thyrotoxicosis-induced Heart Failure.
- Seok Ju Lee, Seung Hwan Lee, Jung Yeon Chin, Youn Mi Song, Sung Won Lee, Min Hee Kim, Mi Ja Kang, Kang Woo Lee, Hyuk Sang Kwon, Kun Ho Yoon, Ho Young Son, Bong Yun Cha
- J Korean Endocr Soc. 2008;23(5):332-336. Published online October 1, 2008
- DOI: https://doi.org/10.3803/jkes.2008.23.5.332
- 1,720 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - Amyloidosis is caused by deposition of insoluble amyloid protein in the extracellular space of organs and tissues. The causes of amyloidosis are classified as primary, secondary, and hereditary, and symptoms develop according to which organ is involved. Cardiac amyloidosis induces cardiomyopathy and is developed by deposition of amyloid proteins in cardiac tissue. We diagnosed a patient with rhabdomyolysis and thyrotoxicosis with underlying Graves' disease 5 years ago. The patient was readmitted recently complaining of general weakness and mild dyspnea, and was diagnosed as relapsed thyrotoxicosis. An echocardiogram was performed for the evaluation of dyspnea and the findings were compatible with infiltrative cardiomyopathy due to amyloidosis. A biopsy of the abdominal subcutaneous fat and rectal mucosa was performed, and diagnosis was amyloidosis with histologic findings. The cause of heart failure was therefore cardiac amyloidosis rather than thyrotoxicosis. This case indicates the importance of evaluating the cause of heart failure in patients with thyrotoxicosis.

- A Case of Pneumocystis Carinii Pneumonia and Cutaneous Nocardiosis Associated with Ectopic ACTH Syndrome.
- Hee Sun Jung, Seung Hwan Lee, Hee Yeon Kim, Eun Ho Chu, Kang Woo Lee, Mi Ja Kang, Ji Hyun Kim, Hyuk Sang Kwon, Kun Ho Yoon, Bong Yun Cha, Ho Young Son
- J Korean Endocr Soc. 2008;23(1):44-50. Published online February 1, 2008
- DOI: https://doi.org/10.3803/jkes.2008.23.1.44
- 1,766 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - Cushing's syndrome is characterized by hypercortisolism and impairment of cell-mediated immune function, increasing the risk of opportunistic infection, as occurs in other immunocompromised groups such as organ transplant recipients, patients with lymphoreticular malignancy, or acquired immunodeficiency syndrome. We report a case of a 68-year-old woman who was affected with pneumocystis carinii pneumonia (PCP) 8 years ago and cutaneous nocardiosis this year. The patient was diagnosed with ectopic ACTH syndrome 8 years ago, but no ectopic ACTH secreting focus was found in radiologic imaging studies. She recovered from PCP and cutaneous nocardiosis after antibiotic (trimethoprim-sulfamethoxazole) administration. After the infection resolved, she underwent laparoscopic bilateral adrenalectomy and was not longer hypercortisolemic.

- Diabetic Ketoacidosis in a Patient with Long-term Clozapine Therapy.
- Youn Joo Jeon, Seung Hwan Lee, Se Na Jang, Eun Sun Kim, Jeong Yo Min, Ji Hyun Kim, Soon Hwa Hong, Jae Hyoung Cho, Hyuk Sang Kwon, Kun Ho Yoon, Bong Yun Cha, Ho Young Son
- J Korean Endocr Soc. 2007;22(5):376-380. Published online October 1, 2007
- DOI: https://doi.org/10.3803/jkes.2007.22.5.376
- 1,785 View
- 20 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - With the broad use of atypical anti-psychotics, altered glucose metabolism has become an item of concern to clinicians and patients. Among the atypical anti-psychotics, clozapine and olanzapine are associated with a relatively high incidence of diabetic ketoacidosis and newly developed diabetes. We report a case of diabetic ketoacidosis in a patient with long-term clozapine therapy. A 35-year-old male with schizophrenia, treated with clozapine for 9 years was admitted into hospital because of comatous mentality. Although never diagnosed with diabetes before, his clinical features were consistent with diabetic ketoacidosis and shock. The patient's serum amylase and lipase levels were elevated and an abdominal computed tomography showed peripancreatic fat infiltration, suggesting the possibility of acute pancreatitis. The patient's serum glucose levels normalized shortly after clozapine treatment. Moreover, the patient ceased all glucose lowering agents upon hospital discharge, and maintained normal blood glucose levels thereafter. As observed in this case, clinicians should carefully screen and monitor blood glucose levels and other clinical parameters in patients treated with atypical anti-psychotics.
-
Citations
Citations to this article as recorded by- Two Cases of Diabetic Ketoacidosis Associated with Paliperidone Treatment in Schizophrenia
Hyun Ho Kim, Hae Kyung Yang, Hyoju Ham, Ho Wook Jeon, Joon Yub Lee, Sea Won Hwang, Bo Hyun Jang, Gi June Min, Jeong Min Lee, Seung-Hwan Lee
The Journal of Korean Diabetes.2014; 15(3): 178. CrossRef - Olanzapine-Induced Diabetic Ketoacidosis and Neuroleptic Malignant Syndrome with Rhabdomyolysis: A Case Report
Young Kyoung Sa, Hyeon Yang, Hee Kyoung Jung, Jang Won Son, Seong Su Lee, Seong Rae Kim, Bong Yeon Cha, Ho Young Son, Chi-Un Pae, Soon Jib Yoo
Endocrinology and Metabolism.2013; 28(1): 70. CrossRef
- Two Cases of Diabetic Ketoacidosis Associated with Paliperidone Treatment in Schizophrenia

- A Patient with Concurrent Medullary and Papillary Carcinoma of the Thyroid.
- Seung Hee Yoo, Keun Joon Lim, Seung Hwan Lee, Ji Hyun Kim, Soon Hwa Hong, Jae Hyoung Cho, Chan Kwon Jung, Hyuk Sang Kwon, Kun Ho Yoon, Min Sik Kim, Bong Yun Cha, Ho Young Son
- J Korean Endocr Soc. 2007;22(3):235-240. Published online June 1, 2007
- DOI: https://doi.org/10.3803/jkes.2007.22.3.235
- 1,876 View
- 19 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - The origin of medullary thyroid carcinoma and papillary thyroid carcinoma are embryogenically different, so these tumors have been thought to be independent of each other. We experienced a case of concurrent medullary and papillary thyroid carcinoma in one patient. The patient underwent total thyroidectomy and both two tumors were located at different lobes, respectively. Both tumors showed their own characteristic pathologic and immunohistochemical findings. The patient's elevated calcitonin level returned to the normal range after operation and there has been no evidence of recurrence. It is still controversial whether the concurrency is just coincidental or it arises from activation of a common tumorigenic pathway.
-
Citations
Citations to this article as recorded by- A Case of Concurrent Papillary and Medullary Thyroid Carcinomas Detected as Recurrent Medullary Carcinoma after Initial Surgery for Papillary Carcinoma
Dongbin Ahn, Jin Ho Sohn, Ji Young Park
Journal of Korean Thyroid Association.2013; 6(1): 80. CrossRef
- A Case of Concurrent Papillary and Medullary Thyroid Carcinomas Detected as Recurrent Medullary Carcinoma after Initial Surgery for Papillary Carcinoma

- A Case of Pituitary Metastasis of Breast Cancer Presenting as Diabetes Insipidus and Panhypopituitarism.
- Jae Wuk Kwak, Byung Soo Jie, Sun Hwa Hong, Ji Hyun Kim, Seung Hwan Lee, Jae Hyung Jo, Hyuk Sang Kwon, Kun Ho Youn, Bong Yun Cha, Ho Young Son
- J Korean Endocr Soc. 2007;22(2):125-129. Published online April 1, 2007
- DOI: https://doi.org/10.3803/jkes.2007.22.2.125
- 2,274 View
- 21 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Metastasis to the pituitary gland from systemic cancer is a rare condition. The breast and lung are the most common sites of primary tumor metastasis. Pituitary metastasis may present with diabetes insipidus, cranial nerve palsy and hypopituitarism, and diabetes insipidus is the most frequent symptom at presentation. We report here on a 44 year-old woman with pituitary metastasis from breast cancer, and she developed central diabetes insipidus and hypopituitarism. The clinical diagnosis was made by performing a water deprivation test, a combined pituitary test and a MRI brain scan, and the latter showed metastatic tumor in the pituitary gland with invasion of the pituitary stalk. Symptomatic relief was obtained with administration of desmopressin; the urine osmolarity was increased with this treatment. We report here on a case of pituitary metastasis from breast cancer and the patient developed central diabetes insipidus and hypopituitarism. We also include a review of the relevant literature.
-
Citations
Citations to this article as recorded by- A Case of Pituitary Metastasis from Breast Cancer That Presented as Left Visual Disturbance
Young Ha Kim, Beom jun Lee, Kyung Jin Lee, Jin Hee Cho
Journal of Korean Neurosurgical Society.2012; 51(2): 94. CrossRef - A Case of Panhypopituitarism and Central Diabetes Insipidus Caused by Primary Central Nervous System Lymphoma
Mi Sun Ahn, Soon Sun Kim, Tae Ho Kim, Seung Jin Han, Dae Jung Kim, Hugh Chul Kim, Se Hyuk Kim, Jae Ho Han, Ho Sung Kim, Yoon-Sok Chung
Journal of Korean Endocrine Society.2008; 23(4): 260. CrossRef
- A Case of Pituitary Metastasis from Breast Cancer That Presented as Left Visual Disturbance


 KES
KES

 First
First Prev
Prev



